 [bctt tweet=”In what have been described as “Medicaid maximization schemes,” states artificially inflate the federal government’s contribution to the Medicaid program while reducing their state share. @SenRonJohnson wants answers. #wiright #wipolitics ” username=”MacIverWisc”]
[bctt tweet=”In what have been described as “Medicaid maximization schemes,” states artificially inflate the federal government’s contribution to the Medicaid program while reducing their state share. @SenRonJohnson wants answers. #wiright #wipolitics ” username=”MacIverWisc”]
MacIver News Service | Sept. 25, 2018
By M.D. Kittle
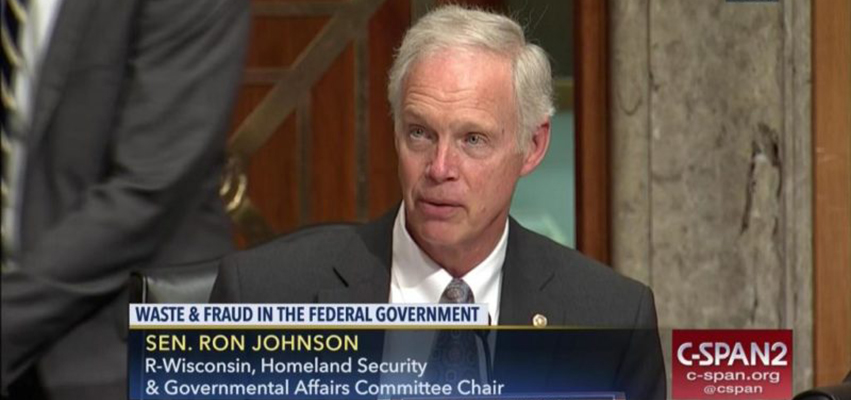
MADISON – U.S. Sen. Ron Johnson wants to know what government officials intend to do about what has been described as “almost limitless” Medicaid funding schemes employed by states, gimmicks that could be costing federal taxpayers hundreds of millions of dollars.
“At a time of rising federal deficits and increased federal Medicaid spending … CMS should closely scrutinize these schemes,” Johnson wrote.
The Oshkosh Republican, who chairs the Senate’s powerful Homeland Security and Governmental Affairs Committee, sent letters last week to the Centers for Medicare and Medicaid Services (CMS) demanding answers to what appears to be state-sectioned shell games with taxpayer money.
“At a time of rising federal deficits and increased federal Medicaid spending … CMS should closely scrutinize these schemes,” Johnson wrote in his letter to CMS Administrator Seema Verma.
The senator’s questions follow last month’s hearing on Medicaid fraud before the Senate committee.
In what have been described as “Medicaid maximization schemes,” states artificially inflate the federal government’s contribution to the Medicaid program while reducing their state share, according to a report by the majority staff of the Homeland Security and Governmental Affairs Committee.
The report is titled, “The Centers For Medicare & Medicaid Services Has Been a Poor Steward of Federal Medicaid Dollars.”
In testimony before the committee last month, U.S. Government Accountability Office Comptroller General Gene Dodaro told members that “the range of (state Medicaid) gimmicks … is almost limitless.”
States and the federal government share Medicaid expenses. The federal obligation varies based on a state’s per capita income. In Wisconsin, the federal government picks up about 60 percent of the Medicaid budget to the state’s 40 percent. The federal contribution, according to the Congressional Research Service, is “open-ended.”
As Dodaro testified, the “open-ended” nature of the federal government’s Medicaid funding obligation incentivizes states to create “all of these types of programs to try to draw down federal dollars.”
Some of the more popular gimmicks, according to Johnson’s letter, include:
- Intergovernmental Transfers (IGTs), which include “transfers of … funds between State and/or local public Medicaid providers and the State Medicaid agency” in ways designed to trigger the release of federal matching funds.
- Provider taxes, in which states tax health care providers and then return the funds to the providers, triggering a federal match.
In one example of questionable transfers, Michigan ‘paid’ $122 million in state funds to county health facilities, along with a $155 million federal match triggered by the state government – and the same day, the county facilities transferred all but $6 million of the $277 million total back to the state,” Johnson wrote, referencing a Government Accountability Office report, on IGT-fostered “State Financing Schemes.” The state “realized a net gain of $149 million over the state’s original outlay of $122 million,” the report found.
More than 40 states impose provider taxes on hospitals, described as a “Medicaid shell game” in December 2017 opinion piece published in the Wall Street Journal.
States have used enhanced federal funds through IGTs “for a range of purposes with no direct link to improving quality of care or increasing Medicaid services,” according to a report from the Inspector General of the U.S. Department of Health and Human Services.
More than 40 states impose provider taxes on hospitals, described as a “Medicaid shell game” in December 2017 opinion piece published in the Wall Street Journal.
Oregon state Rep. Mitch Greenlick, a Democrat from Portland, described the provider tax as a “dream tax.”
“We collect the tax from hospitals, we put it up as a match for federal money, and then we give it back to the hospitals,” Greenlick, chairman of the Legislature’s House Health Care Committee said, as reported by the Portland Tribune. “They have enough money to put people in Medicaid so they have health insurance to pay for hospitalizations.”
While states may use the Medicaid gimmicks at the expense of federal taxpayers, CMS has done a shoddy job at collecting information, according to the General Accounting Office. CMS “generally does not require (or otherwise collect) information from states on the funds they use to finance Medicaid, nor ensure that the data that it does collect are accurate and complete,” GAO noted in its 2015 report. And many state supplemental payments to health care providers, made separately from regular claims-based payments for Medicaid services, are not subject to audits, GAO found.
Johnson has asked the CMS administrator for the agency’s plan to address Medicaid maximization schemes, including proposed actions to hold states and providers accountable for intergovernmental transfers. The senator also wants to know what CMS intends to do about provider taxes used as a Medicaid maximization scheme. And he wants to know why CMS historically has not collected accurate and complete data from states on the sources of funds they use to finance the non-federal Medicaid share.
“Without timely, complete, and accurate data subject to independent audits, CMS and Congress cannot determine the extent of Medicaid maximization schemes and how much they are costing taxpayers,” Johnson said.